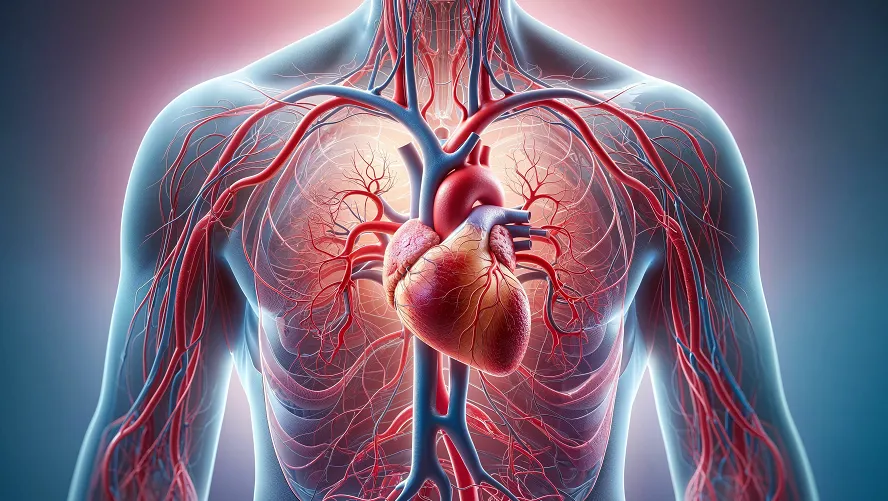
As we age, maintaining healthy blood flow becomes increasingly crucial—and challenging. Poor circulation in seniors isn’t just about cold hands and feet; it can lead to fatigue, slower healing, cognitive fog, and increased risk of heart disease, strokes, or peripheral artery disease (PAD). The good news? Significant improvements are possible with targeted, safe strategies. Here’s your evidence-based guide to boosting circulation and enhancing quality of life for elderly individuals.
Why Circulation Declines with Age?
Aging causes significant changes that impair blood flow. Arteries stiffen (arteriosclerosis) due to elastin loss and collagen buildup, reducing flexibility and increasing blood pressure. Fatty plaque (atherosclerosis) narrows vessel pathways, restricting flow. The heart muscle thickens slightly, reducing its pumping efficiency and cardiac output, especially under stress. Blood vessels produce less nitric oxide, limiting their ability to widen (endothelial dysfunction). Reduced total body water often lowers blood volume, and capillary walls thicken, slowing oxygen/nutrient exchange. These cumulative changes hinder circulation, particularly to extremities and vital organs.
10 Evidence-Backed Strategies to Enhance Blood Flow
Maintaining healthy blood circulation in later years involves evidence-supported approaches: regular gentle movement (like walking or seated exercises) promotes vascular responsiveness; consistent hydration prevents blood thickening; consuming nitrate-rich vegetables (e.g., beets, leafy greens) and omega-3 sources aids vessel dilation. Medical compression wear assists venous return when professionally fitted, while periodic leg elevation reduces edema. Smoking cessation is critical for vascular repair, and rigorous management of conditions like hypertension or diabetes prevents further damage. Gentle massage, contrast hydrotherapy, and maintaining warmth help peripheral flow, and prioritizing 7–8 hours of sleep supports overnight vascular recovery. Always consult a healthcare provider before adjusting routines.
1. Move Consistently (Even Gently!)
Gentle daily movement counteracts age-related circulatory decline by activating the “muscle pump” mechanism. When muscles contract during activities like seated leg lifts or short walks, they compress veins, pushing blood toward the heart. This reduces blood pooling in extremities, lowers venous pressure, and enhances arterial flexibility through nitric oxide release. Aim for 20-30 minutes of low-impact activity daily—split into manageable segments if needed. Water aerobics or tai chi are ideal for joint safety. Always start with a 5-minute warm-up to prevent strain.
Support Tip: Place sticky notes on a wall clock as visual reminders for 10-minute movement breaks every 2 hours.
2. Hydrate Strategically
Aging blunts thirst signals, making dehydration a silent saboteur of circulation. Optimal fluid intake (1.5-2L daily) maintains blood volume and viscosity, preventing sluggish flow that strains the heart. Sip lukewarm water hourly—cold fluids can cause vasospasm. Enhance absorption with electrolyte-rich additions: add a slice of lemon to water or include broth-based soups. Avoid excessive caffeine after noon. Monitor hydration through urine color (pale yellow = ideal).
Support Tip: Use marked water bottles with time-based goals (e.g., “Drink to this line by 10 AM”) to track intake effortlessly.
3. Optimize Nutrition for Vascular Health
Target nutrients combat endothelial dysfunction: Nitrates in beetroot and spinach convert to nitric oxide, dilating arteries. Omega-3s (wild salmon, chia seeds) reduce blood stickiness and arterial plaque. Antioxidants (blueberries, dark chocolate) neutralize free radicals damaging vessel walls. Prioritize potassium-rich foods (avocado, sweet potato) to counter salt-induced hypertension. Limit processed meats and fried foods—their advanced glycation end-products stiffen arteries.
Support Tip: Prep “circulation-booster” snack packs: walnuts + dark cocoa nibs + goji berries for effortless daily doses.
4. Compression Therapy (Under Guidance)
Medical-grade stockings apply graduated pressure (strongest at ankles, decreasing upward) to assist weakened venous valves. This prevents blood backflow and edema by 40-70% in chronic venous insufficiency. Critical: Get professionally measured—ill-fitting stockings can cut off arterial flow. Wear them upon waking (before swelling starts) and remove at night. Hand-wash to maintain elasticity.
Support Tip: Use a stocking donner (silicone tool) and wear rubber gloves for easier application if hand mobility is limited.
5. Elevate Legs Regularly
Gravity-assisted elevation drains stagnant fluid from lower limbs, reducing venous hypertension. Position hips above heart level using wedge pillows for 15-20 minutes post-lunch and dinner. This enhances venous return by ~30%, alleviating swelling and nocturnal cramps. Never elevate over abdominal scars or fresh surgical sites. Breathe deeply during sessions to augment lymphatic flow.
Support Tip: Sync elevation with calming activities: listen to audiobooks or practice diaphragmatic breathing for dual benefits.
6. Quit Smoking (Non-Negotiable)
Nicotine triggers immediate vasoconstriction, spiking blood pressure by 10-15 mmHg within minutes. Long-term, carbon monoxide destroys endothelial cells, accelerating atherosclerosis. Quitting restores nitric oxide production within 8 weeks, improving vessel dilation. Combine cessation aids (patches/lozenges) with cardio exercise to accelerate detox.
Support Tip: Freeze cigarette money daily in a container—after 3 months, use savings for a vascular-friendly reward (e.g., massage).
7. Manage Chronic Conditions Rigorously
Uncontrolled diabetes glycates hemoglobin, starving tissues of oxygen. Hypertension micro-tears arterial linings, inviting plaque. Essential actions: Monitor fasting glucose (<100 mg/dL) and BP (<130/80 mmHg). Take statins/antihypertensives at consistent times. Foot checks prevent unnoticed ulcers—use a mirror for soles.
Support Tip: Create a “health dashboard”: whiteboard with daily meds/logs visible to caregivers for accountability.
8. Massage & Hydrotherapy
Gentle calf massage (5 mins/leg) stimulates superficial veins and lymphatic drainage. Contrast hydrotherapy—alternating 2-min warm (40°C/104°F) and 30-sec cool (18°C/64°F) limb showers—boosts vessel tone adaptability. Never apply ice directly. Dry-brush skin before bathing to enhance surface circulation.
Support Tip: Keep a tennis ball under the desk to roll feet on for passive massage while seated.
9. Keep Warm
Cold exposure triggers peripheral vasoconstriction, reducing blood flow to hands/feet by up to 50%. Maintain core warmth with layers (thermal base + wool mid-layer) and heated mittens/socks. Room temps should stay ≥20°C (68°F). Avoid electric blankets overnight—use pre-warmed rice bags instead.
Support Tip: Place slippers/socks on a heating pad 10 mins before use—cozy footwear encourages mobility.
10. Prioritize Quality Sleep
Deep sleep triggers the “glymphatic surge,” clearing vascular toxins like beta-amyloid. Aim for 7-8 hours in a 18-19°C (65°F) room—coolness optimizes sleep-related BP dip. Untreated sleep apnea causes hypoxia-induced vascular damage; seek CPAP therapy if snoring/gasping occurs.
Support Tip: Use blue-light blocking glasses 2 hours pre-bed to enhance melatonin for deeper restorative sleep.
The Takeaway: It’s Never Too Late
Age-related circulation decline isn’t inevitable. By incorporating consistent movement, heart-healthy nutrition, hydration, and medical management, seniors can significantly improve blood flow, energy levels, mental clarity, and overall well-being. Small, daily actions create powerful ripple effects for vascular health. Empower the elderly in your life to take these steps—consulting their healthcare team along the way—for a more vibrant, active life.







